早期可手术治疗的女性乳腺癌患者术后放疗(苏格兰保乳研究):随机、对照3期研究的30年追踪
以下内容来源于pubmed。
Postoperative radiotherapy in women with early operable breast cancer (Scottish Breast Conservation Trial): 30-year update of a randomised, controlled, phase 3 trial
Abstract
Background: Breast-conserving surgery, adjuvant systemic therapy, and radiotherapy are the standard of care for most women with early breast cancer. There are few reports of clinical outcomes beyond the first decade of follow-up of randomised trials comparing breast-conserving surgery with or without radiotherapy. We present a 30-year update of the Scottish Breast Conservation Trial.
Methods: In this randomised, controlled, phase 3 trial across 14 hospitals in Scotland, women aged younger than 70 years with early breast cancer (tumours ≤4 cm [T1 or T2 and N0 or N1]) were included. They underwent breast-conserving surgery (1 cm margin) with axillary node sampling or clearance. Oestrogen receptor (ER)-rich patients (≥20 fmol/mg protein) received 20 mg oral tamoxifen daily for 5 years. ER-poor patients (<20 fmol/mg protein) received chemotherapy (cyclophosphamide 600 mg/m2, methotrexate 50 mg/m2, and fluorouracil 600 mg/m2 every 21 days intravenously in eight courses). Stratification was by menstrual status (within or more than 12 months from last menstrual period) and ER status (oestrogen concentration ≥20 fmol/mg protein, <20 fmol/mg protein, or unknown) and patients were randomly assigned (1:1) to high-dose (50 Gy in 20-25 fractions) local or locoregional radiotherapy versus no radiotherapy. No blinding was possible due to the nature of the treatment. We report the primary endpoint of the original trial, ipsilateral breast tumour recurrence, and the co-primary endpoint, overall survival. Clinical outcomes were compared by the log-rank test. Hazard ratios (HRs) are reported, with no radiotherapy as the reference group. Failures of the proportional hazards assumption are reported if significant. All analyses are by intention to treat.
Findings: Between April 1, 1985, and Oct 2, 1991, 589 patients were enrolled and randomly assigned to the two treatment groups (293 to radiotherapy and 296 to no radiotherapy). After exclusion of four ineligible patients (two in each group), there were 291 patients in the radiotherapy group and 294 patients in the no radiotherapy group. Median follow-up was 17·5 years (IQR 8·4-27·9). Ipsilateral breast tumour recurrence was significantly lower in the radiotherapy group than in the no radiotherapy group (46 [16%] of 291 vs 107 [36%] of 294; HR 0·39 [95% CI 0·28-0·55], p<0·0001). Although there were differences in the hazard rate for ipsilateral breast tumour recurrence in the first decade after treatment (HR 0·24 [95% CI 0·15-0·38], p<0·0001), subsequent risks of ipsilateral breast tumour recurrence were similar in both groups (0·98 [0·54-1·79], p=0·95). There was no difference in overall survival between the two groups (median 18·7 years [95% CI 16·5-21·5] in the no radiotherapy group vs 19·2 years [16·9-21·3] in the radiotherapy group; HR 1·08 [95% CI 0·89-1 ·30], log-rank p=0·43).
Interpretation: Our findings suggest that patients whose biology predicts a late relapse a decade or more after breast-conserving surgery for early breast cancer might gain little from adjuvant radiotherapy.
Funding: Breast Cancer Institute (part of Edinburgh and Lothian Health Foundation) and PFS Genomics (now part of Exact Sciences).


经常口腔溃疡?常用药物得了解一下,药用对了才好的快


如果锌缺失,会给孩子造成什么危害?


想瘦身却戒不掉主食,放心,有更好的方法


骨髓瘤三期能活多久?


想减肥总是管不住嘴怎么办呢?


甲状腺功能减退症用药注意事项有哪些?


饭后躺下伤身,6件事饭后也尽量不要做


脚气患者的饮食要注意哪些?


斑秃可以治愈么?应该如何治疗?
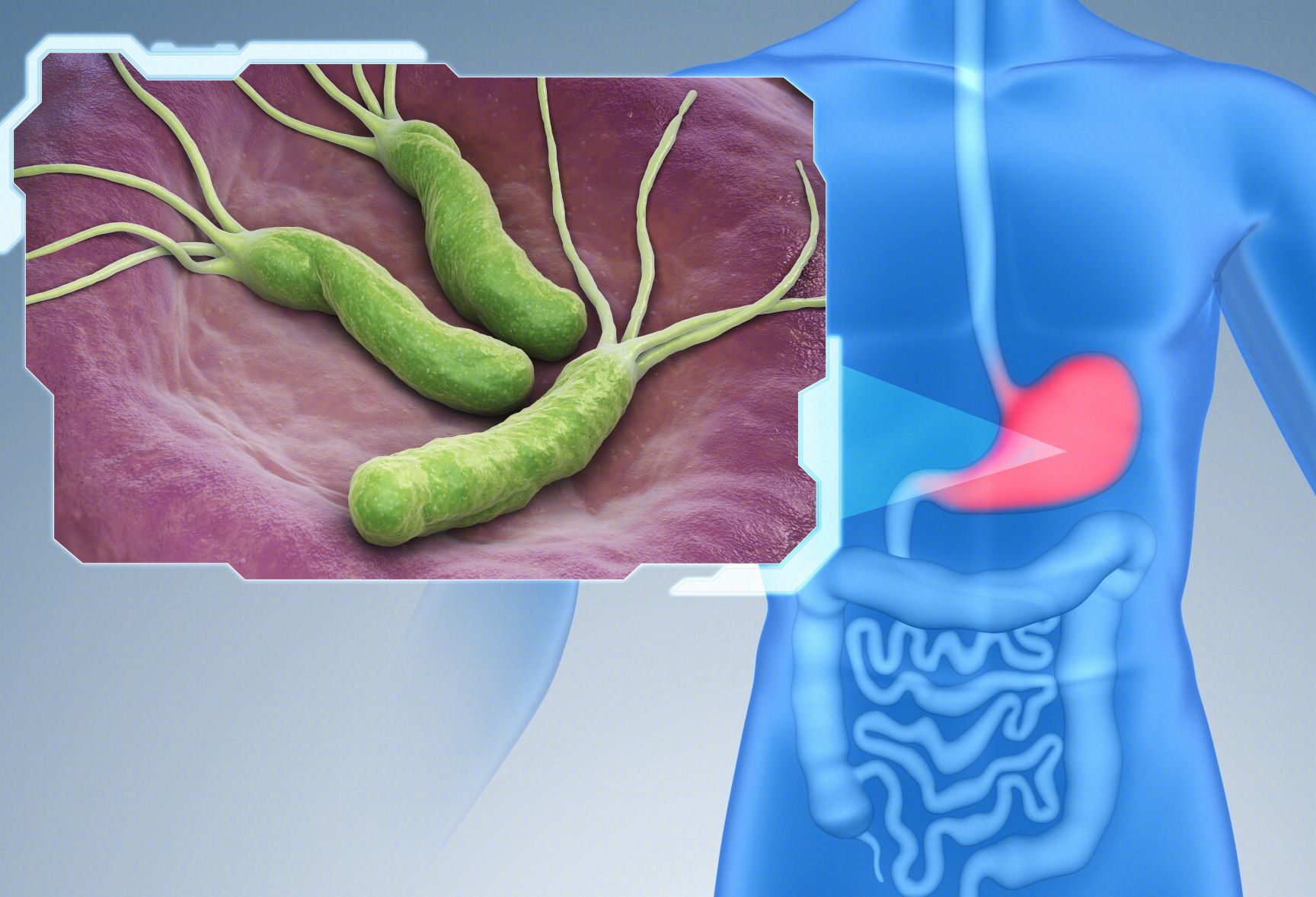
幽门螺杆菌与消化性溃疡




