
乳腺萎缩的原因主要包括年龄因素、雌激素分泌异常、慢性乳腺炎等。
1.年龄因素:随着年龄的增长,女性的性激素水平分泌可出现变化,特别是更年期后,雌激素分泌减少,可导致乳腺组织出现萎缩的现象。
2.雌激素分泌异常:如多囊卵巢综合征、甲状腺功能异常等,这些疾病可导致患者体内的雌激素或黄体酮功能不足。雌激素分泌减少可影响到乳房的生长,进而导致乳腺萎缩的出现,还可伴随着月经不调等症状。
3.慢性乳腺炎:一般是因为急性乳腺炎治疗不当而引起,可导致患者乳房出现肿胀和疼痛感,随着病情的持续存在,也可导致乳腺萎缩的现象。
一旦出现乳房萎缩的情况,需尽快到医院就诊,在医生的指导下进行合理治疗。

切子宫后我会变老吗?
这是一个绝大多数得了妇科疾病需要通过切子宫治疗女性最关心的问题,肯定的是,切除子宫后,妇女两种功能就丧失了:一是不会再有月经,二是不能怀孕生育。对于这两种情况,准备手术的女性都能理解。实际上,很多女性担心的是宫切除后会迅速变老吗?影响性生活吗?会变成男的吗?
子宫切除后会变老吗?这主要取决于切除子宫时是否同时切除卵巢。子宫只是生殖道的器官之一,卵巢才是分泌性激素的器官,当卵巢功能衰退后,女性就进入更年期,月经也就停止了。因此,对于卵巢功能正常的妇女,如果切除子宫时保留卵巢,通常不会加快更年期的到来。术后除了不再来月经之外,卵巢会象术前一样分泌激素并作用于外阴、阴道、乳房等器官,所以不会出现乳房萎缩、阴道干涩及潮热、出汗、烦躁等症状。但是如果切除子宫时同时切除卵巢,确会很快出现更年期症状。但是可以通过妇科内分泌医生的指导下适当给予激素补充治疗,缓解症状并预防骨质疏松症。
子宫切除术影响性生活吗?实际上经过测量统计,除非恶性肿瘤需切除较长的阴道外,子宫全切术后的阴道长度与手术前基本相同,所以不会对性交造成障碍。从前认为宫颈在性交过程中对润滑阴道起一定作用,经过深入研究也被否定了。如果卵巢保留,仍会有雌激素产生。如果卵巢也一起切除,由于雌激素的缺乏,会出现乳房萎缩、阴道干涩及性欲下降等,会对性生活造成一定影响,通过补充外源性雌激素可有效改善症状。
子宫切除后会变成男的吗?切除了子宫后绝不会变成男的!因为子宫只是卵巢的下级器官,卵巢对女性的形体保持有决定作用。而且,即使切除了双侧卵巢,同样不会变成男的。

成年女性到一定年龄后(尤其是哺乳后)很多都会出现乳房不同程度的下垂情况,虽然不影响健康,但会严重影响形体美,严重者也会影响日常生活(如很多下垂严重者,乳房下皱璧易发生湿疹、糜烂等)。现就介绍一下乳房下垂的常见原因。
1.产后荷尔蒙的变化造成乳房萎缩。
2.体重的突然减少,也即体型由"胖"到"瘦"。
3.乳房皮肤组织松弛。
4.乳房体积过于肥大,也即"巨乳症",由于乳房体积过大过重,长时期的重力作用必然导致下垂。
正常成年女性的乳房,乳房下皱璧与乳房下极是在同一平面。如低于此平面就属于下垂。通常可根据下垂程度分 4 种类型:
- 轻度下垂:乳房下极超过下皱璧 1-2cm。
- 中度下垂:乳房下极超过下皱璧 2-3cm。
- 重度下垂:乳房下极超过下皱璧 4-10cm。
- 特重度下垂:乳房下极超过下皱璧 10cm 以上。

(Nipple)左右各一,位于第2~4肋间,女性不光是哺乳,而且是性感和形体美的标志。
分为颈部、体部和基底部,的直径正常情况下约10mm表的高度为 7~8mm,临床上直径大于10mm,就称为过大,头长度大于8mm,就称为过高,另外临床上还有表现为颈部短或缺失的扁平,直径小于8mm的小,由于先天因素或后天因素引起的内陷和缺失等,这些都是常见的疾病,除了影 响美观、性感和形体美之外,还可能对相应的功能造成影响。

(图一:正常左,内陷右)
由15-20个乳管、平滑肌、致密的结缔组织(Cooper韧带)和丰富的感觉神经末梢所组成,其血供主要来于胸乳内外侧动脉的分支,有深支和浅支供应,行手术时在底部(乳晕)做环形的切口千万不要切得太深,完全离断其深支和浅支动脉,造成坏死。支配的神经来于肋间神经的皮支。
由于社会的发展和进步,人们越来越重视健康与美丽,原先未予重视的疾病、缺陷等门诊病例逐渐增多,很多女性朋友要求整形处理诸如左右的不对称、过大、过小、内陷、过高等问题,同时由于乳腺恶性肿瘤保乳手术开展越来越多,先天性、外伤性等原因造成的(甚至乳晕)缺失患者要求恢复及乳晕复合体,除矫正 形体美,更重要的是树立自信心,因此开展及乳晕再造手术的病人也越来越多。

(图一:正常左,内陷右)
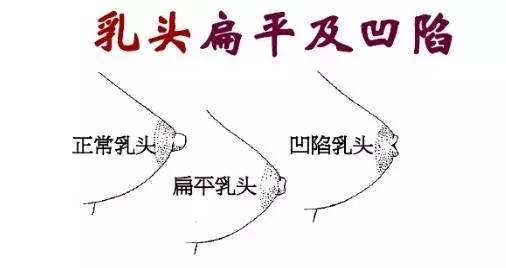
(图二:正常左 扁平中 凹陷右)

2

3

不需保留乳腺管的乳头内陷手术,是采用乳头中间纵行切口切至乳头底部并横向延长切口至 乳晕,也可采用乳晕弧形切口游离至乳头底部,彻底分离切断挛缩、粘连的维束,切断乳管,这时底部往往十分薄弱和空虚,需采用转移的翻转三角皮瓣缝合填充或采用^物$料如 脱细胞异体真皮填充,近年来多报道乳头底部填充后再采用荷包缝合,进一步让乳头突出,但注意的是荷包打结不要太紧,防止乳头缺血。
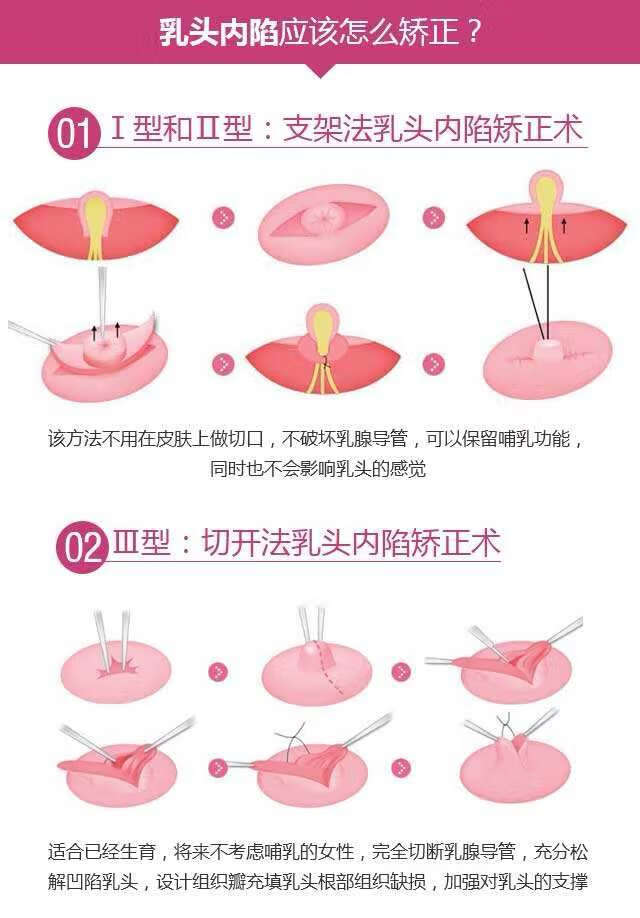
(图四:一、二、三型乳头内陷的治疗方法)
保留乳管的乳头内陷手术,这一方式要相当有经验的医师手术,所有的游离、分离均保 留乳管,原则上只切断乳头底部挛缩、粘连的纤维束,过短的乳管切断其粘连后让其伸直, 发育引起的乳管过短若确实影响手术效果,可部分切断,该手术十分细致,其最大的并发症 是内陷改善和乳头伸直效果有局限性,但临床报道其治疗效果满意。

(图五:乳头内陷的手术治疗)
值得注意的是临床上常常会面临几个乳头问题的同时整形矫正,如乳头过大伴有乳头过 长;乳头内陷伴有乳头过小等,其手术切口和手术方式及功能都要有所兼顾,并注意乳房大小和左右对称性。
乳头内陷具体手术方法:
手术具体步骤:乳头缝线牵引上提乳头。于乳晕区横、纵两个方向贯穿乳头基底走“井”字形用3号尼龙线作“U”缝合,远离乳头基底部缝线走行于皮下,打结线结埋于皮下。
乳头内陷手术并发症除感染、血肿、切口裂开等一般手术并发症外,乳头凹陷手术还有如下并发症:

以下内容来源于新英格兰医学杂志。
Presentation of Case

Differential Diagnosis
Movement Disorders
Seizures
Functional Movement Disorder
Dyskinesia
Limb-Shaking TIAs
Clinical Impression and Initial Management

Clinical Diagnosis
Dr. Albert Y. Hung’s Diagnosis
Pathological Discussion

Pathological Diagnosis
Additional Management
Final Diagnosis

以下内容来源于新英格兰医学杂志。
Presentation of Case
Dr. Christine M. Parsons (Medicine): A 75-year-old woman was evaluated at this hospital because of arthritis, abdominal pain, edema, malaise, and fever.
Three weeks before the current admission, the patient noticed waxing and waning “throbbing” pain in the right upper abdomen, which she rated at 9 (on a scale of 0 to 10, with 10 indicating the most severe pain) at its maximal intensity. The pain was associated with nausea and fever with a temperature of up to 39.0°C. Pain worsened after food consumption and was relieved with acetaminophen. During the 3 weeks before the current admission, edema developed in both legs; it had started at the ankles and gradually progressed upward to the hips. When the edema began to affect her ambulation, she presented to the emergency department of this hospital.
A review of systems that was obtained from the patient and her family was notable for intermittent fever, abdominal bloating, anorexia, and fatigue that had progressed during the previous 3 weeks. The patient reported new orthopnea and nonproductive cough. Approximately 4 weeks earlier, she had had diarrhea for several days. During the 6 weeks before the current admission, the patient had lost 9 kg unintentionally; she also had had pain in the wrists and hands, 3 days of burning and dryness of the eyes, and diffuse myalgias. She had not had night sweats, dry mouth, jaw claudication, vision changes, urinary symptoms, or oral, nasal, or genital ulcers.
The patient’s medical history was notable for multiple myeloma (for which treatment with thalidomide and melphalan had been initiated 2 years earlier and was stopped approximately 1 year before the current admission); hypothyroidism; chikungunya virus infection (diagnosed 7 years earlier); seropositive erosive rheumatoid arthritis affecting the hands, wrists, elbows, and shoulders (diagnosed 3 years earlier); vitiligo; and osteoarthritis of the right hip, for which she had undergone arthroplasty. Evidence of gastritis was reportedly seen on endoscopy that had been performed 6 months earlier. Medications included daily treatment with levothyroxine and acetaminophen and pipazethate hydrochloride as needed for cough. The patient consumed chamomile and horsetail herbal teas. She had no known allergies to medications, but she had been advised not to take nonsteroidal antiinflammatory drugs after her diagnosis of multiple myeloma.
Approximately 5 months before the current admission, the patient had emigrated from Central America. She lived with her daughter and grandchildren in an urban area of New England. She had previously worked in health care. She had no history of alcohol, tobacco, or other substance use. There was no family history of cancer or autoimmune, renal, gastrointestinal, pulmonary, or cardiac disease.
On examination, the temporal temperature was 37.1°C, the heart rate 106 beats per minute, the blood pressure 152/67 mm Hg, and the oxygen saturation 100% while the patient was breathing ambient air. She had a frail appearance and bitemporal cachexia. The weight was 41 kg and the body-mass index (the weight in kilograms divided by the square of the height in meters) 15.2. Her dentition was poor; most of the teeth were missing, caries were present in the remaining teeth, and the mucous membranes were dry. She had abdominal tenderness on the right side and mild abdominal distention, without organomegaly or guarding. Bilateral axillary lymphadenopathy was palpable. Infrequent inspiratory wheezing was noted.
The patient had swan-neck deformity, boutonnière deformity, ulnar deviation, and distal hyperextensibility of the thumbs (Fig. 1). Subcutaneous nodules were observed on the proximal interphalangeal joints of the second and third fingers of the right hand and on the proximal interphalangeal joint of the fourth finger of the left hand. Synovial thickening of the metacarpophalangeal joints of the second fingers was noted. There was mild swelling and tenderness of the wrists. She had pain with flexion of the shoulders and right hip, and there was subtle swelling of the shoulders and right knee. Pitting edema (3+) and vitiligo were noted on the legs. No sclerodactyly, digital pitting, telangiectasias, appreciable calcinosis, nodules, nail changes (including pitting), or tophi were present. The remainder of the examination was normal.

The blood levels of glucose, alanine aminotransferase, aspartate aminotransferase, bilirubin, globulin, lactate, lipase, magnesium, and phosphorus were normal, as were the prothrombin time and international normalized ratio; other laboratory test results are shown in Table 1. Urinalysis showed 3+ protein and 3+ blood, and microscopic examination of the sediment revealed 5 to 10 red cells per high-power field and granular casts. Urine and blood were obtained for culture. An electrocardiogram met (at a borderline level) the voltage criteria for left ventricular hypertrophy.

Dr. Rene Balza Romero: Computed tomography (CT) of the chest, abdomen, and pelvis, performed after the intravenous administration of contrast material, revealed scattered subcentimeter pulmonary nodules (including clusters in the right middle lobe and patchy and ground-glass opacities in the left upper lobe), trace pleural effusion in the left lung, coronary and valvular calcifications, and trace pericardial effusion, ascites, and anasarca. The scans also showed slight enlargement of the axillary lymph nodes (up to 11 mm in the short axis) bilaterally and a chronic-appearing compression fracture involving the T12 vertebral body.
Dr. Parsons: Morphine and lactated Ringer’s solution were administered intravenously. On the second day in the emergency department (also referred to as hospital day 2), the blood levels of haptoglobin, folate, and vitamin B12 were normal; other laboratory test results are shown in Table 1. A rapid antigen test for malaria was positive. Wright–Giemsa staining of thick and thin peripheral-blood smears was negative for parasites; the smears also showed Döhle bodies and basophilic stippling. Antigliadin antibodies and anti–tissue transglutaminase antibodies were not detected. Tests for hepatitis A IgG and hepatitis C antibodies were positive. Tests for hepatitis B core and surface antibodies were negative. A test for human immunodeficiency virus type 1 (HIV-1) and type 2 (HIV-2) was negative.
Findings on abdominal ultrasound imaging performed on the second day (Fig. 2A and 2B) were notable for a small volume of ascites and kidneys with echogenic parenchyma. Ultrasonography of the legs showed no deep venous thrombosis. An echocardiogram showed normal ventricular size and function, aortic sclerosis with mild aortic insufficiency, moderate tricuspid regurgitation, a right ventricular systolic pressure of 39 mm Hg, and a small circumferential pericardial effusion. Intravenous hydromorphone was administered, and the patient was admitted to the hospital.

On the third day (also referred to as hospital day 3), nucleic acid testing for cytomegalovirus, Epstein–Barr virus, and hepatitis C virus was negative, and a stool antigen test for Helicobacter pylori was negative. An interferon-γ release assay for Mycobacterium tuberculosis was also negative. Oral acetaminophen and ivermectin and intravenous hydromorphone and furosemide were administered.
Dr. Balza Romero: Radiographs of the hands (Fig. 2C through 2F) showed joint-space narrowing of both radiocarpal joints and proximal interphalangeal erosions involving both hands. Radiographs of the shoulders showed arthritis of the glenohumeral joint and alignment suggestive of a tear of the right rotator cuff. A radiograph of the pelvis showed diffuse joint-space narrowing of the left hip, without osteophytosis, and an intact right hip prosthesis.
Dr. Parsons: Diagnostic tests were performed, and management decisions were made.
Differential Diagnosis
Cancer
Infectious Disease
Autoimmune Disease
Hypocomplementemia
Dr. Beth L. Jonas’s Diagnosis
Pathological Discussion
Pathological Diagnosis
Discussion of Management
Follow-up
Final Diagnosis
Overlap syndrome of rheumatoid arthritis and systemic lupus erythematosus complicated by proliferative lupus nephritis, superimposed on amyloid A amyloidosis.

以下内容来源于PubMed。
Abstract
Sacituzumab govitecan (SG) significantly improved progression-free survival (PFS) and overall survival (OS) versus chemotherapy in hormone receptor-positive human epidermal growth factor receptor 2-negative (HR+HER2-) metastatic breast cancer (mBC) in the global TROPiCS-02 study. TROPiCS-02 enrolled few Asian patients. Here we report results of SG in Asian patients with HR+HER2- mBC from the EVER-132-002 study. Patients were randomized to SG (n = 166) or chemotherapy (n = 165). The primary endpoint was met: PFS was improved with SG versus chemotherapy (hazard ratio of 0.67, 95% confidence interval 0.52-0.87; P = 0.0028; median 4.3 versus 4.2 months). OS also improved with SG versus chemotherapy (hazard ratio of 0.64, 95% confidence interval 0.47-0.88; P = 0.0061; median 21.0 versus 15.3 months). The most common grade ≥3 treatment-emergent adverse events were neutropenia, leukopenia and anemia. SG demonstrated significant and clinically meaningful improvement in PFS and OS versus chemotherapy, with a manageable safety profile consistent with prior studies. SG represents a promising treatment option for Asian patients with HR+HER2- mBC (ClinicalTrials.gov identifier no. NCT04639986 ).

以下内容来源于PubMed。
Abstract
Irritable bowel syndrome with diarrhea (IBS-D) is a common and chronic gastrointestinal disorder that is characterized by abdominal discomfort and occasional diarrhea. The pathogenesis of IBS-D is thought to be related to a combination of factors, including psychological stress, abnormal muscle contractions, and inflammation and disorder of the gut microbiome. However, there is still a lack of comprehensive analysis of the logical regulatory correlation among these factors. In this study, we found that stress induced hyperproduction of xanthine and altered the abundance and metabolic characteristics of Lactobacillus murinus in the gut. Lactobacillus murinus-derived spermidine suppressed the basal expression of type I interferon (IFN)-α in plasmacytoid dendritic cells by inhibiting the K63-linked polyubiquitination of TRAF3. The reduction in IFN-α unrestricted the contractile function of colonic smooth muscle cells, resulting in an increase in bowel movement. Our findings provided a theoretical basis for the pathological mechanism of, and new drug targets for, stress-exposed IBS-D.
Keywords: AdorA2B; Lactobacillus murinus; irritable bowel syndrome with diarrhea; spermidine; stress; type I interferon; xanthine.

以下内容来源于PubMed。
Abstract
The severe bronchiolitis endotype characterized by a high abundance of H. influenzae, high proportion of RV-A and RV-C infections, and high asthma genetic risk had a significantly higher risk for developing asthma.
Background: Infants with bronchiolitis are at increased risk for developing asthma. Growing evidence suggests bronchiolitis is a heterogeneous condition. However, little is known about its biologically distinct subgroups based on the integrated metagenome and asthma genetic risk signature and their longitudinal relationships with asthma development.
Methods: In a multi-center prospective cohort study of infants with severe bronchiolitis (i.e., bronchiolitis requiring hospitalization), we profiled nasopharyngeal airway metagenome and virus at hospitalization, and calculated the polygenic risk score of asthma. Using similarity network fusion clustering approach, we identified integrated metagenome-asthma genetic risk endotypes. We also examined their longitudinal association with the risk of developing asthma by age six years.
Results: Of 450 infants with bronchiolitis (median age, 3 months), we identified five distinct endotypes-characterized by their nasopharyngeal metagenome, virus, and asthma genetic risk profiles. Compared with endotype A infants (who clinically resembled "classic" bronchiolitis), endotype E infants (characterized by a high abundance of H. influenzae, high proportion of RV-A and RV-C infections, and high asthma genetic risk) had a significantly higher risk for developing asthma (35.9% versus 16.7%; ORadj, 2.24; 95%CI, 1.02-4.97; p=0.046). The pathway analysis showed that endotype E had enriched microbial pathways (e.g., glycolysis, L-lysine, arginine metabolism) and host pathways (e.g., IFNs, IL-6/JAK/STAT3, fatty acids, MHC, and immunoglobin-related) (FDR<0.05). Additionally, endotype E had a significantly higher proportion of neutrophils (FDR<0.05).
Conclusion: In this multi-center prospective cohort study of infant bronchiolitis, the clustering analysis of integrated-omics data identified biologically distinct endotypes with differential risks for developing asthma.
以下内容来源于PubMed。
Summary
Background
Methods
Findings
Interpretation
Funding
Keywords
展开更多















