乌鲁木齐市友谊医院
中医心身医学科
简介:乌鲁木齐市友谊医院,又称乌市第三人民医院,始建于1948年,历经59年风雨洗礼,现已发展成为乌鲁木齐市一所集医疗、预防、教学、保健、康复为一体的综合性三级甲等医院。医院拥有四家分院,是爱婴医院、卫生部“国际紧急救援中心”和“亚洲紧急救援中心”定点医院,同时也是新疆医科大学临床医学院、自治区全科医师培训中心实践教学基地和新疆石河子医学院教学医院。 在众多科室中,中医心身医学科独树一帜。该科室致力于为患者提供全方位的心身疾病诊疗服务,拥有经验丰富的医生团队。目前,中医心身医学科医生数量虽不多,但专家阵容强大,为患者提供专业、优质的医疗服务。科室擅长治疗社交恐怖、轻躁狂等疾病,为广大患者带来了福音。 乌鲁木齐市友谊医院中医心身医学科,秉承着“以患者为中心”的服务理念,为广大患者提供温馨、舒适的就医环境,致力于打造区域医疗品牌的典范。在这里,患者可以享受到全方位、多层次的健康保障。



好评99%
接诊量682
平均等待-
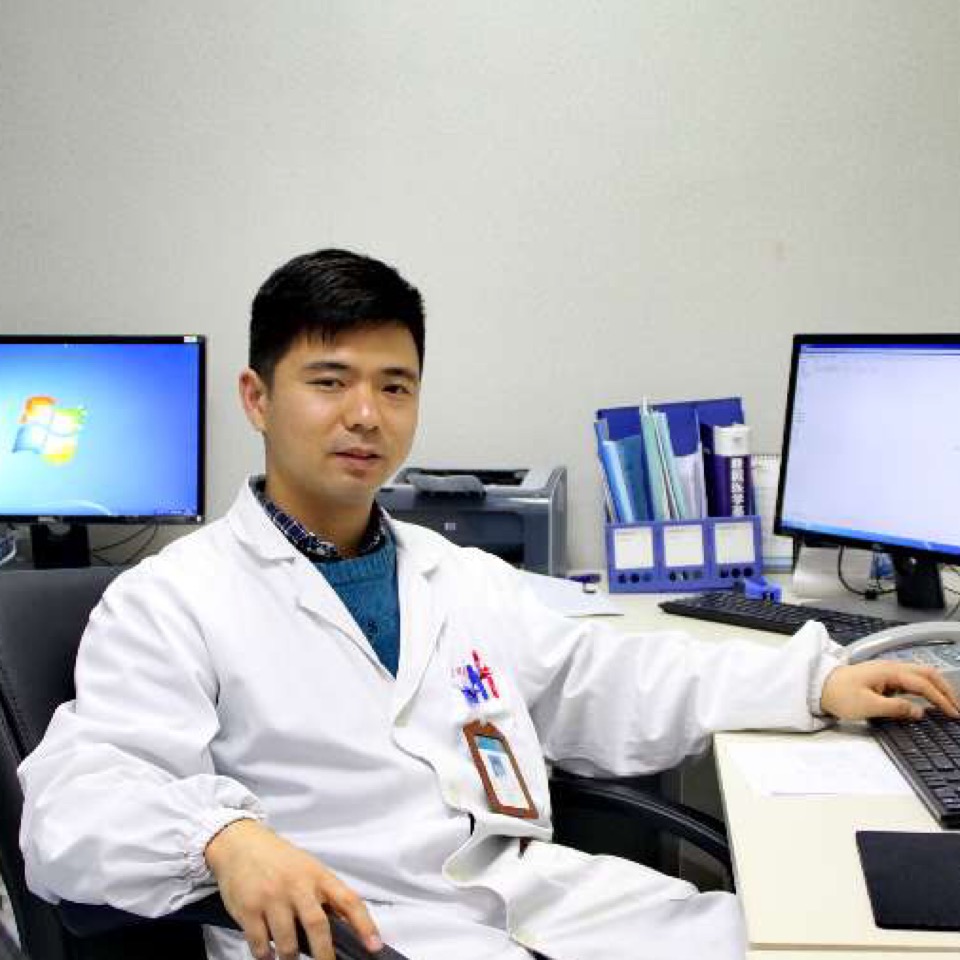
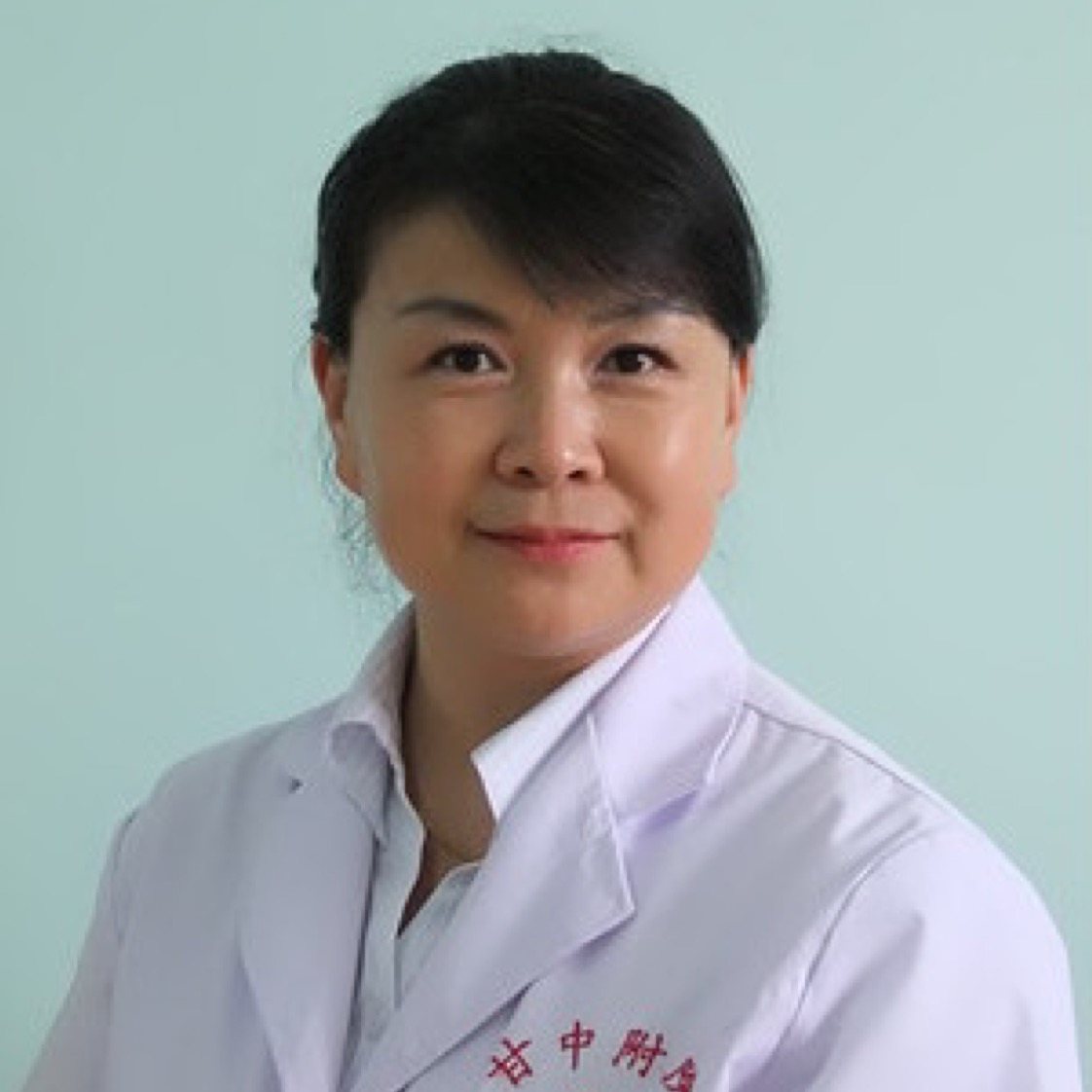
擅长:专业领域:精神疾病的诊断治疗,心理问题的疏导及治疗,婚姻危机干预,青少年厌学及自信心训练,人际关系疏导等。
{肝气郁结} 2例}
{精神异常} 1例}
{神经衰弱} 1例}

好评-
接诊量27
平均等待7小时
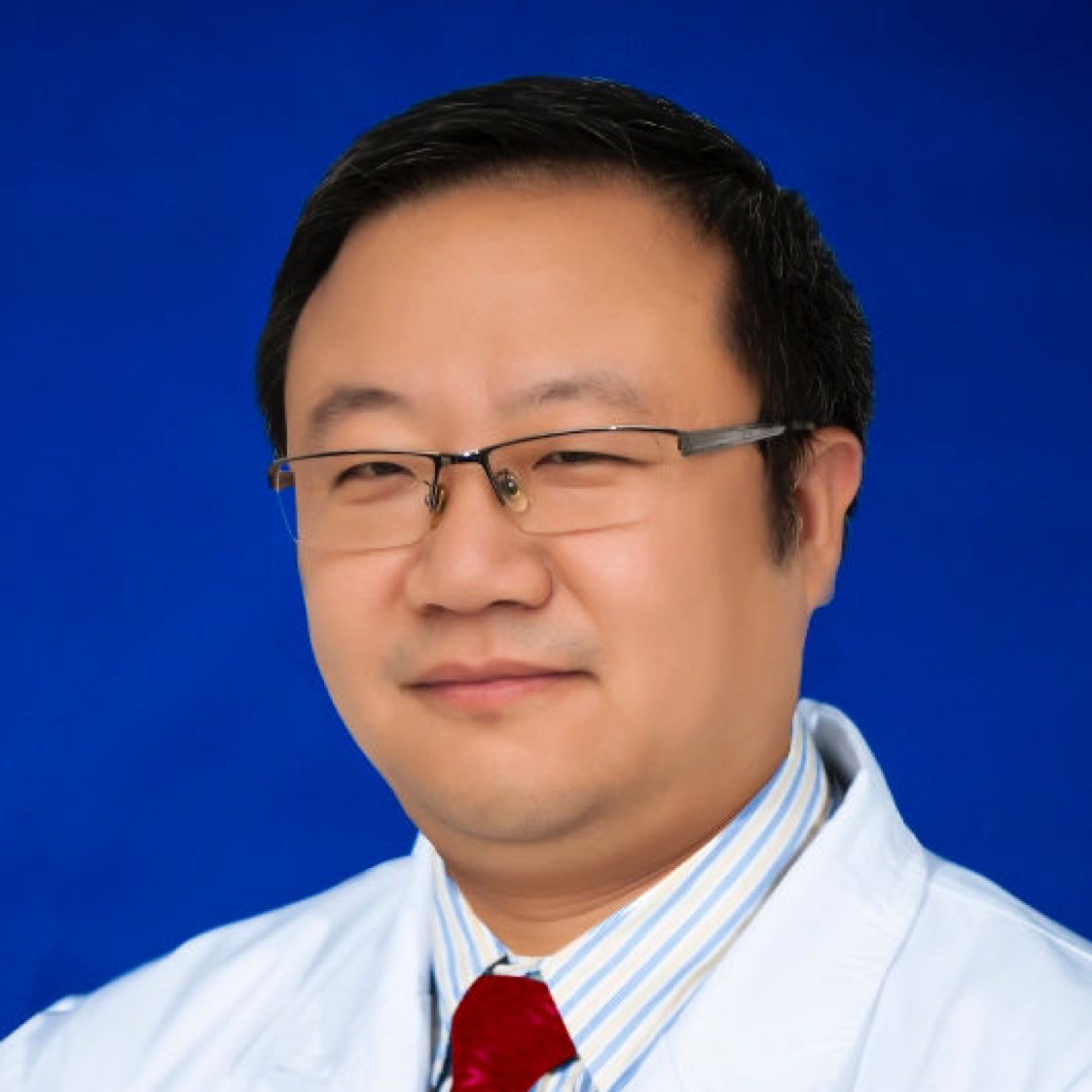
擅长:1.睡眠障碍、神经衰弱、焦虑症、应激障碍、植物神经功能紊乱、更年期综合征、强迫症、心身疾病等轻性精神疾病的诊断和中西医结合治疗; 2.抑郁症、躁狂症、双相障碍、脑器质性精神障碍,精神分裂症、使用酒精所致精神障碍等重性精神疾病的诊断和中西医结合治疗; 3.各种心理问题:婚恋困扰、亲子关系、夫妻关系、人际关系、性心理障碍等。 4.擅长精神科药物的临床应用。熟悉多种心理治疗方法、心理测查及各种精神科常用评定量表的理论和技术知识;并在疑难及有躯体合并症的精神疾病等方面积累了较多经验。 5.擅长精神疾病的早期识别和干预



好评100%
接诊量3
平均等待-
擅长:擅长运用中西医结合及心理干预的方法对失眠、抑郁、焦虑、头痛、眩晕、植物神经功能紊乱、神经衰弱等心身疾病及精神障碍进行诊治;用认知重建及中医五行音乐进行心理干预。
乌鲁木齐市友谊医院中医心身医学科疾病推荐专家
新疆乌鲁木齐市中医心身医学科疾病推荐专家
科普文章