
普通感冒
以鼻咽部黏膜炎症为主要临床表现,包括咳嗽、流涕、打喷嚏、鼻塞等症状。
早期症状主要以鼻部炎症为主,可有喷嚏、鼻塞、流清水样鼻涕,初期可有咽部不适或咽干,咽痒或烧灼感。
2~3 天后变为稠涕,可有咽痛或声嘶,有时由于咽鼓管炎可出现听力减退,也可出现流泪、味觉迟钝、呼吸不畅、咳嗽、少量咳痰等症状。
一般无发热及全身症状,或仅有低热。严重者除发热外,可感乏力不适、畏寒、四肢酸痛和头痛及食欲不振等全身症状。
医生检查可见鼻腔黏膜充血、水肿、有分泌物,咽部轻度充血,胸部检查多无异常。
以咽炎
为主的上感
急性病毒性咽炎
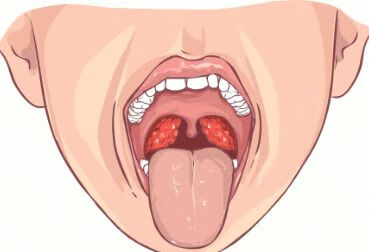
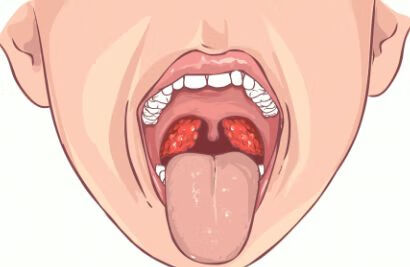
临床主要表现为咽部发痒和灼热感,咳嗽少见,可有发热和乏力。医生检查可见咽部明显充血、水肿,颌下淋巴结肿痛。

咽炎,临床上的常见病多发病,很多人可能对其也并不陌生,咽炎通常是由病毒、细菌感染引起,其常见的临床表现有咽部灼热感,咽喉疼痛,咽部充血水肿,咽干,咽痒咳嗽,嗓子有痰不易咳出,咽部异物感等等。那么咽炎和支气管哮喘有关系吗?咽炎会引起支气管哮喘吗?今天我们来共同探讨一下。
首先,我们来了解一下支气管哮喘,支气管哮喘是由多种细胞和细胞组分参与的以气道慢性炎症为特征的疾病,而且这种慢性炎症通常认为与气道高反应性有关,从而导致出现广泛、多变的可逆性呼气气流受限。支气管哮喘临床症状通常是反复发作的喘息、气促、胸闷和(或)咳嗽等。所以,不管是从发病机制还是临床症状来看,支气管哮喘和咽炎都没有必然的联系。当然长期的慢性咽炎,呼吸道反复感染,以及变应性咽炎是有可能合并支气管哮喘的。咽炎和支气管哮喘发病原因不同,其治疗也就不同,咽炎通常我们需要抗炎,清热解毒,注意休息,营养支持等治疗。而支气管哮喘我们通常需要服用糖皮质激素,抗胆碱能药物,β2受体激动剂的药物,茶碱类药物,白三烯调节剂等药物治疗。
总而言之,一般来说,咽炎和支气管哮喘并没有必然的联系,不管是从发病机制,还是临床症状来看,咽炎和支气管哮喘都是不同的疾病,其治疗原则也就不同。
在这不平凡的 8 月下旬,来了一位主诉咽痛的中年患者,看似简单的咽炎,实则暗藏玄机!
患者,男,40 岁,主诉咽痛半年就诊。期间在当地多家医院就诊,均以咽炎治之,效果不佳,遂来我院门诊耳鼻喉科就诊。电子喉镜检查可见上颚布满簇状疱疹样物,咽后壁充血(++)。由于第一次见,没经验,还以为是疱疹性咽炎,故请来主任帮忙诊断,经验丰富的主任立即怀疑是其他疾病引起,主任说上颚面并不是疱疹,像疣状物多一点,并开具传染病三项检查,抽血发现梅毒抗体异常升高。
梅毒在我国近年来有逐年蔓延的趋势,耳鼻咽喉科是性器官以外较为常见的发病部位,我国报道较少,大部分为二期梅毒,具有极强的直接和间接传染的特点。它起病较为隐匿,患者常隐瞒病史,易被漏诊。临床特点是,发病年龄以中青年为多,多有不洁性生活史。一期梅毒:好发于扁桃体,称为扁桃体硬下疳,占生殖器外硬下疳的 7.5%。而上述病例患者应属二期梅毒了。二期梅毒的表现为:患者约有 36.3%发生咽梅毒。病程一般 2 个月到半年,甚至可长达 2 年。咽梅毒病变可累及腭弓、扁桃体、悬雍垂、软腭、咽后壁等处,且累及部位粘膜充血,表面可见暗红色斑丘疹和暗红色黏膜斑。
综上所述,本例患者应考虑为二期咽梅毒,此病于耳鼻咽喉头颈外科属特殊相关疾病。

婴儿咽炎大多数与受凉感冒、呼吸道炎症感染等等因素有关系,临床上按症状分为以下:1、急性咽炎,大多数是由于病毒或者细菌感染所诱发导致,患者多出现咽部疼痛感,由于疼痛导致患者不喜欢说话、不喜欢动、不喜欢吃东西,经常流口水,经常出现哭闹,精神状态比较萎靡,临床上检查的时候能看到咽部充血,双侧扁桃体充血等等相关症状。部分患者病变严重的时候容易出现急性喉炎,从而出现声音嘶哑、喉喘鸣等等相关症状。2、慢性咽炎,慢性咽炎症状一般不典型,有的患者多有反复的清嗓子,反复干咳,经常有咽干,总感觉嗓子有东西等等相关症状,部分患者也可以出现反复用手抠嗓子等等相关症状。总之,婴儿咽炎的症状,家属要做好定期观察,家属可以

婴儿急性喉炎的最佳治疗方案包括以下:第一、如果婴儿出现了喉阻塞症状,首选应用激素,比如应用地塞米松肌注或者静脉滴注治疗,能够减轻喉部组织的肿胀,使患者喉阻塞得到解除。第二、抗炎治疗,需要尽早应用有效的足量的抗生素,控制感染,首选静脉输液治疗。第三、支持疗法,由于婴儿体质的特殊性,对婴儿出现急性喉炎的情况,要注意婴儿水电解质平衡,要注意保护心脏的功能,避免发生急性心衰等等相关的表现。第四、婴儿急性喉炎的时候,要尽量减少哭闹,使婴儿能够安静休息,以免导致婴儿出现呼吸困难加重。第五、婴儿出现急性喉炎,如果出现了重度喉阻塞,比如三度或者三度以上的喉阻塞,可以考虑进行气管切开或者做气管插管等紧急救治治疗。
如今患癌症的人较多,且有年轻化的趋势,以至于有些人有点头痛脑热、咳嗽咽痛的就联想到癌症。
据统计,我国有60-70%的人有不同程度的咽炎。首先明确地回答,慢性咽炎并不会癌变!
慢性咽炎是咽炎中的一种,常常是由于急性咽炎反复发作发作而导致的,主要症状是:咽喉干、痒、有异物感、咽不下去也咳不出来的感觉,严重的患者还会产生咽喉疼痛,恶心等症状。
咽喉炎,急性与慢性有什么不同?
急性咽喉炎大部分是和病原体(病毒、细菌)的感染有关,是上呼吸道感染的一种,这种病变大部分是可以通过抗感染治疗后完全恢复。
但慢性咽喉炎不同,不能完全根治,会反复发作。慢性咽喉炎是由长期的非生物因素刺激所致,比如长期用嗓过度、经常进食辛辣刺激的食物、不断地吸入有毒有害物质或者工业粉尘所引起的。咽喉部常常有充血红肿,咽后壁有淋巴滤泡增生等慢性炎症表现。
这样的改变基本上不能完全恢复正常,局部敏感不耐受刺激,无论哪种刺激,超过平常能耐受的范围都会加重咽喉部的炎症反应。
长期咽炎会发展为喉癌?
这个不用担心,慢性咽炎并不是癌前病变,单纯的慢性咽炎不会发生癌变。无论咽部症状有多复杂或者与他人不同的症状,都不会发生癌变,而且对身体其他脏器和部位没有明显的影响。
目前的文献记载和临床观察,还没有慢性咽炎导致肿瘤的报道。但如果合并有增生性喉炎则要注意,增生性喉炎属于癌前病变,因喉部粘膜细胞长期的增生,细胞有导致癌变的可能。
如何缓解慢性咽炎?
慢性咽炎既然不会癌变,只要从生活上、饮食上注意,从情绪上进行调整,适当使用局部药物,完全可以缓解症状。
生活上,戒烟是充当其冲的,长期抽烟的人没有一个不合并慢性咽炎的。此外,酒精对咽喉部刺激也很大,尤其是高度酒,有慢性咽炎的人最好不要饮酒。
平时不要接触有刺激性气体的东西,厨房要通风,减少油烟刺激,开空调时室内使用加湿器。
饮食上应该多吃一些清淡的易消化的食物,不要吃辛辣,刺激,油腻及过咸的食物,多吃新鲜的蔬菜和水果,平时多喝水滋润咽喉部。
慢性咽炎虽不会导致癌变的发生,但的的确确会给平时的生活带来一定的麻烦,主观症状比较多,所以平时多调理和保养,尽量让症状消失,不让其反复发作。

轻度喉咙疼一般是不会癌变的,这种及时治疗的话,一般是可以好转的。但是重度的喉咙疼患者,如果不休息喉咙的保养,是有可能癌变的。喉咙疼主要是因为平时不良的生活饮食习惯,经常性的吃一些辛辣刺激性的食物所引起的。这些都会引起咽喉部黏膜的刺激,从而引起喉咙的发炎疼痛。出现这种症状的话,可以买些川贝枇杷膏喝,或者是熬一些冰糖雪梨汤喝,都可以减轻这种症状。同时要调整自己的生活饮食习惯,不要吸烟喝酒,也不要经常性的吃一些辛辣,刺激,上火的食物,保持一个清淡的饮食。

第一步“看大小”
怎么看肿大的程度呢?记住 2 个标记,第一是咽腭弓,第二是中线。
- 如果扁桃体肿大,但没超过咽腭弓,就是一度肿大;
- 超过咽腭弓,二度肿大;
- 肿大越过中线,跑到对侧,甚至两个扁桃体紧贴在一起,那铁定是三度肿大啦。
在儿童 6-9 月龄前,腭扁桃体未发育,一般无法看到。过了婴儿期,扁桃体一旦发育完全,可能会在整个儿童期保持肿大的状态。所以这里可以推翻有两个常见的错误:
- 儿童时期的扁桃体肿大,并无太大意义。
比如下图,就是一个我从四年级放学的孩子里找出来的扁桃体,二度肿大,但她没有任何咽痛、咳嗽、发热、打呼噜妨碍呼吸等情况,她妈妈说一年内只因“感冒”去过 2 次医院,完全不存在“慢性扁桃体炎”之说。
所谓感染,一般伴有炎症反应,也就是“红肿热痛”。短期内没有快速增大或者极不对称,单纯稳定的肿大是正常现象,请保持淡定,安心观察,渡过儿童期。
第二步:看分泌物
当扁桃体上有白色物质的时候,要仔细分辨。强调一点,不是所有扁桃体上的白点点,都是化脓。这里常见的有 3 种情况:
- 细菌感染: A 组链球菌也称为化脓性链球菌,是儿童和青少年细菌性咽炎最常见的病原体,约占所有扁桃体炎的 30%,也就是需要用抗生素的类型。
- 病毒感染:病毒感染占所有咽炎的绝大部分,接近 60%,但有分泌物的常见为 EB 病毒感染,少数为 CMV,也就是巨细胞病毒感染,两者均能引起传染性单核细胞增多症。这类属于病毒感染,抗生素治疗无效。
可以从扁桃体渗出物,判别是否为细菌性化脓性扁桃体炎。
因 EB 病毒而起的扁桃体、往往是灰灰的、均质的一层膜,早期厚一些,恢复期薄一些。而化脓性的扁桃体炎,有一种多中心的集落感。
另外,细菌感染局部还有一个非常有趣的特点,那就是满天星一样的出血点,往往是链球菌溶血素、透明质酸酶共同作用的结果,有这种情况,不管血象高不高,都提示细菌,特异性非常高。
要是分不清怎么办呢?这就需要医生结合全身症状来判断。如果您吃不准,请来医院就诊。
扁桃体结石:慢性扁桃体感染时,扁桃体隐窝可滋生细菌。隐窝内可能会形成细菌的“尸体”、黏液和其他碎片构成的钙化性结石。扁桃体结石可能会有恶臭,并可引起口臭,也有可能没有味道;可能较大甚至如黄豆,也有稍小如小米。
这个时候,应该准备好棉签或者镊子、手电筒轻轻压,一般可以压得出来,但是容易出血。如果自己实在拿不出,请来医院就诊。
第三步:看全身状况
- 细菌性扁桃体炎往往发热且伴有怕冷或者寒战、头痛、疲乏,学龄期儿童较多;可有全身的鸡皮样猩红热皮疹,咽部易化脓和出血点。
- 细菌性扁桃体炎可以引发周围脏器的炎症,比如扁桃体周围蜂窝织炎和脓肿,可能出现重度咽痛、发热、声音含混、流涎、张口困难和/或颈痛,尤其是颈部周围红肿,必须立即来医院就诊。
- 病毒性如鼻病毒、冠状病毒、埃可病毒、柯萨奇病毒等的临床特征包括合并结膜炎、清鼻涕或者打喷嚏、声音嘶哑、散在的溃疡病变、病毒疹和/或腹泻。EB 病毒引起的传染性单核细胞增多症往往除了咽部表现以外,还有颈部淋巴结肿大、眼睑水肿和外周血淋巴细胞增多(注意不是单核细胞)。
- 其他如扁桃体结石,往往见于反复扁桃体感染、饮食重口味、卫生习惯差甚至不定期刷牙的孩子,在无症状的间歇期发现的单发为主的白色不痛白色分泌物,往往较深、不伴有全身症状。

以下内容来源于新英格兰医学杂志。
Presentation of Case

Differential Diagnosis
Movement Disorders
Seizures
Functional Movement Disorder
Dyskinesia
Limb-Shaking TIAs
Clinical Impression and Initial Management

Clinical Diagnosis
Dr. Albert Y. Hung’s Diagnosis
Pathological Discussion

Pathological Diagnosis
Additional Management
Final Diagnosis

以下内容来源于新英格兰医学杂志。
Presentation of Case
Dr. Christine M. Parsons (Medicine): A 75-year-old woman was evaluated at this hospital because of arthritis, abdominal pain, edema, malaise, and fever.
Three weeks before the current admission, the patient noticed waxing and waning “throbbing” pain in the right upper abdomen, which she rated at 9 (on a scale of 0 to 10, with 10 indicating the most severe pain) at its maximal intensity. The pain was associated with nausea and fever with a temperature of up to 39.0°C. Pain worsened after food consumption and was relieved with acetaminophen. During the 3 weeks before the current admission, edema developed in both legs; it had started at the ankles and gradually progressed upward to the hips. When the edema began to affect her ambulation, she presented to the emergency department of this hospital.
A review of systems that was obtained from the patient and her family was notable for intermittent fever, abdominal bloating, anorexia, and fatigue that had progressed during the previous 3 weeks. The patient reported new orthopnea and nonproductive cough. Approximately 4 weeks earlier, she had had diarrhea for several days. During the 6 weeks before the current admission, the patient had lost 9 kg unintentionally; she also had had pain in the wrists and hands, 3 days of burning and dryness of the eyes, and diffuse myalgias. She had not had night sweats, dry mouth, jaw claudication, vision changes, urinary symptoms, or oral, nasal, or genital ulcers.
The patient’s medical history was notable for multiple myeloma (for which treatment with thalidomide and melphalan had been initiated 2 years earlier and was stopped approximately 1 year before the current admission); hypothyroidism; chikungunya virus infection (diagnosed 7 years earlier); seropositive erosive rheumatoid arthritis affecting the hands, wrists, elbows, and shoulders (diagnosed 3 years earlier); vitiligo; and osteoarthritis of the right hip, for which she had undergone arthroplasty. Evidence of gastritis was reportedly seen on endoscopy that had been performed 6 months earlier. Medications included daily treatment with levothyroxine and acetaminophen and pipazethate hydrochloride as needed for cough. The patient consumed chamomile and horsetail herbal teas. She had no known allergies to medications, but she had been advised not to take nonsteroidal antiinflammatory drugs after her diagnosis of multiple myeloma.
Approximately 5 months before the current admission, the patient had emigrated from Central America. She lived with her daughter and grandchildren in an urban area of New England. She had previously worked in health care. She had no history of alcohol, tobacco, or other substance use. There was no family history of cancer or autoimmune, renal, gastrointestinal, pulmonary, or cardiac disease.
On examination, the temporal temperature was 37.1°C, the heart rate 106 beats per minute, the blood pressure 152/67 mm Hg, and the oxygen saturation 100% while the patient was breathing ambient air. She had a frail appearance and bitemporal cachexia. The weight was 41 kg and the body-mass index (the weight in kilograms divided by the square of the height in meters) 15.2. Her dentition was poor; most of the teeth were missing, caries were present in the remaining teeth, and the mucous membranes were dry. She had abdominal tenderness on the right side and mild abdominal distention, without organomegaly or guarding. Bilateral axillary lymphadenopathy was palpable. Infrequent inspiratory wheezing was noted.
The patient had swan-neck deformity, boutonnière deformity, ulnar deviation, and distal hyperextensibility of the thumbs (Fig. 1). Subcutaneous nodules were observed on the proximal interphalangeal joints of the second and third fingers of the right hand and on the proximal interphalangeal joint of the fourth finger of the left hand. Synovial thickening of the metacarpophalangeal joints of the second fingers was noted. There was mild swelling and tenderness of the wrists. She had pain with flexion of the shoulders and right hip, and there was subtle swelling of the shoulders and right knee. Pitting edema (3+) and vitiligo were noted on the legs. No sclerodactyly, digital pitting, telangiectasias, appreciable calcinosis, nodules, nail changes (including pitting), or tophi were present. The remainder of the examination was normal.

The blood levels of glucose, alanine aminotransferase, aspartate aminotransferase, bilirubin, globulin, lactate, lipase, magnesium, and phosphorus were normal, as were the prothrombin time and international normalized ratio; other laboratory test results are shown in Table 1. Urinalysis showed 3+ protein and 3+ blood, and microscopic examination of the sediment revealed 5 to 10 red cells per high-power field and granular casts. Urine and blood were obtained for culture. An electrocardiogram met (at a borderline level) the voltage criteria for left ventricular hypertrophy.

Dr. Rene Balza Romero: Computed tomography (CT) of the chest, abdomen, and pelvis, performed after the intravenous administration of contrast material, revealed scattered subcentimeter pulmonary nodules (including clusters in the right middle lobe and patchy and ground-glass opacities in the left upper lobe), trace pleural effusion in the left lung, coronary and valvular calcifications, and trace pericardial effusion, ascites, and anasarca. The scans also showed slight enlargement of the axillary lymph nodes (up to 11 mm in the short axis) bilaterally and a chronic-appearing compression fracture involving the T12 vertebral body.
Dr. Parsons: Morphine and lactated Ringer’s solution were administered intravenously. On the second day in the emergency department (also referred to as hospital day 2), the blood levels of haptoglobin, folate, and vitamin B12 were normal; other laboratory test results are shown in Table 1. A rapid antigen test for malaria was positive. Wright–Giemsa staining of thick and thin peripheral-blood smears was negative for parasites; the smears also showed Döhle bodies and basophilic stippling. Antigliadin antibodies and anti–tissue transglutaminase antibodies were not detected. Tests for hepatitis A IgG and hepatitis C antibodies were positive. Tests for hepatitis B core and surface antibodies were negative. A test for human immunodeficiency virus type 1 (HIV-1) and type 2 (HIV-2) was negative.
Findings on abdominal ultrasound imaging performed on the second day (Fig. 2A and 2B) were notable for a small volume of ascites and kidneys with echogenic parenchyma. Ultrasonography of the legs showed no deep venous thrombosis. An echocardiogram showed normal ventricular size and function, aortic sclerosis with mild aortic insufficiency, moderate tricuspid regurgitation, a right ventricular systolic pressure of 39 mm Hg, and a small circumferential pericardial effusion. Intravenous hydromorphone was administered, and the patient was admitted to the hospital.

On the third day (also referred to as hospital day 3), nucleic acid testing for cytomegalovirus, Epstein–Barr virus, and hepatitis C virus was negative, and a stool antigen test for Helicobacter pylori was negative. An interferon-γ release assay for Mycobacterium tuberculosis was also negative. Oral acetaminophen and ivermectin and intravenous hydromorphone and furosemide were administered.
Dr. Balza Romero: Radiographs of the hands (Fig. 2C through 2F) showed joint-space narrowing of both radiocarpal joints and proximal interphalangeal erosions involving both hands. Radiographs of the shoulders showed arthritis of the glenohumeral joint and alignment suggestive of a tear of the right rotator cuff. A radiograph of the pelvis showed diffuse joint-space narrowing of the left hip, without osteophytosis, and an intact right hip prosthesis.
Dr. Parsons: Diagnostic tests were performed, and management decisions were made.
Differential Diagnosis
Cancer
Infectious Disease
Autoimmune Disease
Hypocomplementemia
Dr. Beth L. Jonas’s Diagnosis
Pathological Discussion
Pathological Diagnosis
Discussion of Management
Follow-up
Final Diagnosis
Overlap syndrome of rheumatoid arthritis and systemic lupus erythematosus complicated by proliferative lupus nephritis, superimposed on amyloid A amyloidosis.
展开更多









